A strong corticosteroid used for a number of ailments requiring quick and strong effects is hydrocortisone. In endocrine disorders, it effectively manages primary and secondary adrenocortical insufficiency by restoring hormonal balance and alleviating symptoms. In collagen diseases like systemic lupus erythematosus, it reduces inflammation and modulates immune responses, improving patient outcomes.
The drug is also crucial in treating severe dermatological conditions such as Stevens-Johnson syndrome, as well as allergic reactions like bronchial asthma and anaphylaxis. Additionally, it addresses gastrointestinal diseases, including ulcerative colitis and Crohn’s disease, and is vital in emergencies, particularly in treating shock related to adrenal insufficiency.
Healthcare providers may administer Solnac by intravenous injection, intravenous infusion, or intramuscular injection. Importantly, intravenous injection is the preferred method for initial emergency use. Furthermore, healthcare providers should assess the patient’s condition to determine the most suitable route of administration for subsequent doses. Additionally, this ensures that the treatment aligns with the patient’s needs. After the initial emergency period, healthcare providers should then consider using a longer-acting injectable preparation or an oral preparation for ongoing treatment. Additionally, this allows for better management of the patient’s condition over time.
Dosage usually ranges from 100 mg to 500 mg, depending on the severity of the condition, and is administered by intravenous injection over a period of one to ten minutes. Moreover, healthcare providers should closely monitor the patient during this time to assess the effectiveness of the treatment. Additionally, adjusting the dosage may be necessary based on the patient’s response. Additionally, the healthcare provider may repeat this dose at intervals of 2, 4, or 6 hours based on the patient’s response and clinical condition. Furthermore, this approach allows for tailored treatment that effectively addresses the patient’s needs.
Dosage requirements must be personalized according to the specific disease being treated, the severity of the condition, and the patient’s response during the entire treatment period. Healthcare providers must make a risk/benefit decision for each individual case on an ongoing basis.
Healthcare providers should determine the proper maintenance dosage by gradually decreasing the initial drug dosage in small increments at appropriate time intervals until they reach the lowest dosage that maintains an adequate clinical response.
In general, healthcare providers should continue high-dose corticosteroid therapy only until the patient’s condition stabilizes, usually not beyond 48 to 72 hours. If healthcare providers must continue hydrocortisone therapy beyond 48 to 72 hours, they should be aware that hypernatremia may occur. Therefore, it may be preferable to replace Solnac with a corticosteroid like methylprednisolone sodium succinate, which causes little or no sodium retention.
If healthcare providers decide to stop the drug after long-term therapy, they need to withdraw it gradually rather than abruptly.
Healthcare providers can effectively minimize undesirable effects by using the lowest effective dose for the shortest duration necessary. Furthermore, they should recognize that corticosteroid therapy serves as an adjunct to, and not a replacement for, conventional therapy. Additionally, this approach ensures comprehensive patient care while addressing specific needs.
In patients with liver disease, healthcare providers may consider reduced dosing due to the potential for an increased effect.
Paediatric population: Healthcare providers should reduce the dosage for infants and children, prioritizing the severity of the condition and the patient’s response over age or size. Furthermore, they should closely monitor the patient’s response to ensure effectiveness and adjust the dosage as needed. Additionally, this approach helps ensure safety while addressing the unique needs of pediatric patients. Dosage should not be less than 25 mg daily.
Elderly patients: Healthcare providers may administer Solnac by intravenous injection, intravenous infusion, or intramuscular injection. Notably, intravenous injection is the preferred method for initial emergency use. Additionally, healthcare providers should evaluate the patient’s needs to determine the most appropriate method of administration in subsequent treatments. After the initial emergency period, healthcare providers should then consider using a longer-acting injectable preparation or an oral preparation for continued treatment.
Preparation of solutions: For intravenous or intramuscular injection prepare the solution aseptically by adding not more than 10 ml of sterile water for injections to the contents of one vial of Solnac 500 mg, shake and withdraw for use.
For intravenous infusion, healthcare providers should first prepare the solution by adding no more than 10 ml of sterile water for injections to the vial. Healthcare providers can then add this solution to 100 ml to 1000 ml of 5% dextrose in water (or isotonic saline solution, or 5% dextrose in isotonic saline solution if the patient is not on sodium restriction).
When reconstituted as directed, the pH of the solution will range from 7.0 to 8.0.
Healthcare providers do not recommend administering this medicine via the intrathecal route.
The incidence of predictable undesirable side effects associated with corticosteroid use, including hypothalamic-pituitary-adrenal suppression, correlates with several factors: specifically, the relative potency of the drug, the dosage, the timing of administration, and the duration of treatment. Moreover, such side effects include: Very common (≥1/10), Common (≥1/100 to <1/10), Uncommon (≥1/1,000 to <1/100), Rare (≥1/10,000 to <1/1,000), Very rare (<1/10,000), Not known (cannot be estimated from the available data).
Frequency: Not Known
Infections and Infestations
Patients may experience opportunistic infections and other infections.
Blood and Lymphatic System Disorders
Patients may develop leucocytosis.
Immune System Disorders
Patients may have drug hypersensitivity, which can lead to an anaphylactic reaction or an anaphylactoid reaction.
Endocrine Disorders
Patients may present with Cushingoid facies, hypopituitarism, or steroid withdrawal syndrome.
Metabolism and Nutrition Disorders
Patients may experience metabolic acidosis, sodium retention, fluid retention, hypokalaemic alkalosis, and dyslipidaemia.
Psychiatric Disorders
Patients may suffer from affective disorders, psychotic disorders, or mental disorders.
Eye Disorders
Patients may develop central serous chorioretinopathy, cataracts, glaucoma, exophthalmos, or blurred vision.
Cardiac Disorders
Patients may experience congestive heart failure.
Respiratory, Thoracic and Mediastinal Disorders
Patients may develop pulmonary embolism or experience hiccups.
Gastrointestinal Disorders
Patients may suffer from peptic ulcers, abdominal distension, oesophageal ulceration, or acute pancreatitis.
Reproductive System and Breast Disorders
Patients may experience irregular menstruation or amenorrhoea.
Healthcare providers must exercise particular care when considering the use of systemic corticosteroids in patients with the following conditions, and they need to monitor patients frequently:
1. Osteoporosis: Healthcare providers should exercise caution when using corticosteroids in patients with osteoporosis, especially since long-term use and large doses of glucocorticoids generally associate with osteoporosis, putting post-menopausal females at particular risk.
2. Hypertension: This condition warrants caution when using corticosteroids.
3. Severe Affective Disorders: A history of severe affective disorders, especially previous steroid psychosis, necessitates careful consideration.
4. Diabetes: Corticosteroids, including hydrocortisone, can increase blood glucose levels, worsen pre-existing diabetes, and predispose those on long-term corticosteroid therapy to diabetes mellitus, particularly with a family history of diabetes.
5. Tuberculosis: A history of tuberculosis, whether existing or in the patient’s past, requires special care.
6. Glaucoma: Therefore, healthcare providers should closely monitor patients with glaucoma or a family history of glaucoma.
7. Corticosteroid-Induced Myopathy: Consequently, a previous history of this condition requires caution in corticosteroid use.
8. Liver Failure or Cirrhosis: Therefore, patients with these conditions need careful assessment.
9. Renal Insufficiency: Healthcare providers should exercise caution when prescribing corticosteroids to these patients.
10. Epilepsy: Requires special attention when using corticosteroids.
11. Peptic Ulceration: Therefore, healthcare providers should consider this condition carefully.
12. Fresh Intestinal Anastomoses: As a result, healthcare providers should exercise caution with these patients.
13. Thrombophlebitis: Thus, a predisposition to this condition necessitates monitoring.
14. Pyogenic Infections: Consequently, patients with abscesses or other pyogenic infections require careful monitoring.
15. Ulcerative Colitis: For this reason, this condition needs special consideration.
16. Diverticulitis: Accordingly, close monitoring is necessary.
17. Myasthenia Gravis: Hence, healthcare providers should carefully assess patients with this condition.
18. Exanthematous Diseases: Healthcare providers should exercise caution when considering corticosteroids for these patients.
Store below 30°C. Protected from light.
Healthcare providers should use the reconstituted solution immediately. Additionally, they should ensure that any unused solution is stored properly to maintain its effectiveness. Furthermore, they must be aware of the recommended storage conditions if immediate use is not possible. If not used, store it for 24 hours at 2°C to 8°C under aseptic conditions. If not used immediately, in-use storage times and conditions are the responsibility of the user.
Keep the medicine out of reach of children.
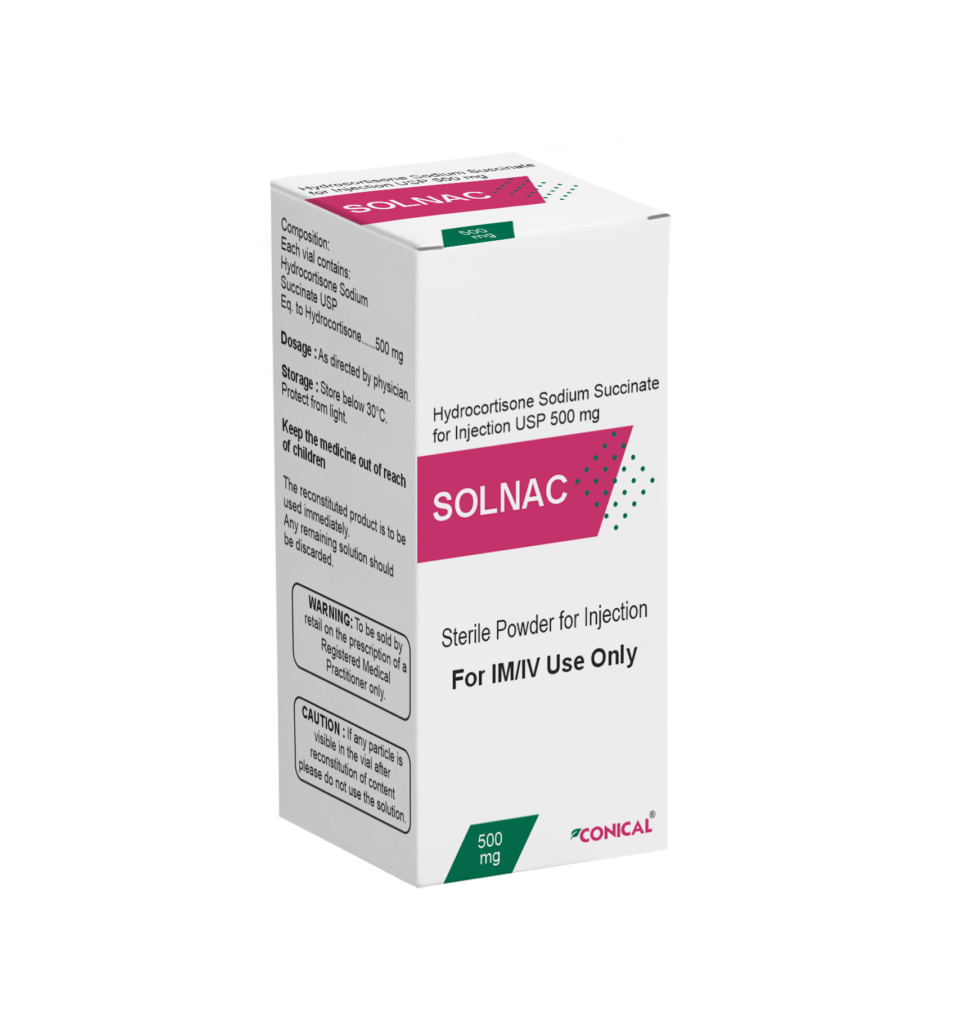
The 10 ml clear molded glass vial features a grey bromobutyl rubber stopper and is sealed with an orange flip-off aluminum seal. Furthermore, the injection solution of hydrocortisone sodium succinate USP 500 mg is provided in this glass vial. Additionally, the vial is packaged within a unit carton that includes a pack insert for user reference.
Contact us directly to receive full information on the product, the formulation, the science behind it, stability data, and more. Our Business Development Manager is a click away.
Conical Pharmaceuticals is a professionally managed and dynamic organization with decades of experience in the pharmaceutical field. With a desire of providing opportunities for a better life, we work very hard to bring quality drugs to our customers. We have instilled a level of trust and confidence amongst our clients by supplying the best quality products.